Don’t know where the “sinuses” are but I know they hurt.
One of the 10 most common diagnoses in ambulatory practice is “Acute Rhinosinusitis” AKA “Sinusitis”. Interestingly, it is the fifth most common diagnosis for which antibiotics are prescribed. 1, 2 Most people know about “sinus pain”, and a great deal take over the counter medications to try to treat “sinus pain”. In my short career, I have come across a fair bit of interesting explanations of what and where the sinuses actually are. Some people think it’s attached to the brain while others feel that it’s just within the nasal passage.
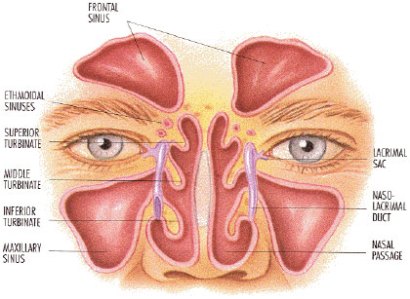
The above picture notes the three sinuses we usually look for, including the frontal, ethmoidal, sphenoidal and maxillary sinuses. Commonly, rhinitis (inflammation of the nasal passages) and sinusitis (inflammation of the sinus cavity) are affected at the same time and as such, the more preferable naming is rhinosinusitis.
Most commonly the sinuses affected are maxillary and ethmoidal and having isolated frontal or sphenoidal sinus is quite rare. It should be noted that 90% of upper respiratory infections are accompanied by viral rhinosinusitis.
The great majority (98-99.5%) of patients do not get bacterial superinfections, which is why many times sinusitis does not require the use of antibiotics. There are many guidelines regarding this and is the main reason there are more physicians recommending against the use antibiotics for uncomplicated, mild-moderate rhinosinusitis. 2
Most common causes of rhinosinusitis include:
1. Viral sources (Most common) – rhinovirus, coronavirus, influenza A and B, parainfluenza, respiratory syncytial virus, adenovirus and enterovirus.
2. Bacterial source – Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis
3. Allergens
4. Local Irritants
It is important to note that the majority of cases of rhinosinusitis are caused by viruses. As such, most cases of acute rhinosinusitis resolve without treatment (SORT A, Cochrane review, The Cochrane Library 2011 Issue 3).
It is important to monitor for possible signs of acute bacterial infection (i.e. purulent nasal discharge, maxillary tooth ache, unilateral facial pain or maxillary sinus tenderness). In addition, there is a concept of “double sickening”, where patients get sick then improve and then worsen again. These patients need to be assessed as possibly having a bacterial infection.
If these are not present and the course has been less than 10 days, acute viral rhinosinusitis is usually diagnosed. This education is usually given to the patient, which is important so that patients do not feel that they are being brushed off, go to a walk in clinic and are given antibiotics for no other reason than to have the patient leave the clinic.
As such, an algorithm that I commonly use in my practice is as below:
The American Board of Internal Medicine Foundation and American Academy of Allergy, Asthma & Immunology have an initiative called Choosing Wisely, which discuss whether antibiotics should be used for sinusitis and the other expensive things that have been done for sinusitis without evidence (i.e. CT scans for acute rhinosinusitis).
It is also part of my colleague and current Ontario College of Family Physician President Dr. Frank Martino’s MAIN-PRO C lecture – “Don’t Just Do Something, Stand There!”
Patients can be great advocates for decreasing use of antibiotics, and in turn decreasing financial burden on the system. Most antibiotics aren’t very expensive but unnecessary use has driven up healthcare cost to the tune of approximately of 30 million dollars a year.
Sinuses are one of those very small things in the body that can hurt the most and its funny how there are so many people who still think that the word sinuses refers to a condition rather than mucus and membrane lined cavities found in the skull. This article has been quite informative…